The landscape of patient care and payment models is evolving faster than ever.
How can we best adapt and lead our organizations into the future?
The answer lies in embracing digital transformation to transition from the traditional health care model toward value-based care. Let's break down this journey.
A Blast from the Past: Fee-for-Service
Understanding Fee-for-Service
Fee-for-Service (FFS) is as traditional as it comes. With this model, healthcare providers charge for every individual service they offer. A patient visits, receives treatment—be it a blood test, an x-ray, or a consultation—and the provider bills for each of those services.
The Good and the Not-So-Good of FFS
In the FFS model, the simplicity is its biggest advantage. It’s a tried and true method. Everyone involved, from the patient to the insurance company, understands the process.
However, the model is not without its downsides. Its main pitfall is that it tends to prioritize the volume of services over their value. The more tests, procedures, or consultations a provider schedules, the more they earn. Take, for instance, our fictional patient Mrs. Smith, who routinely sees her doctor for recurrent back pain. Under FFS, rather than exploring long-term pain management or preventative strategies, she might undergo repeated MRIs purely because they're billable. This system doesn’t always prioritize Mrs. Smith's best interests.
The New Kid on the Block: Value-Based Care (VBC)
The Essence of VBC
Value-based care is a fresh perspective on healthcare. It emphasizes the quality of care over the number of services provided. So, instead of billing for every single service, providers are rewarded based on patient outcomes and overall care quality.
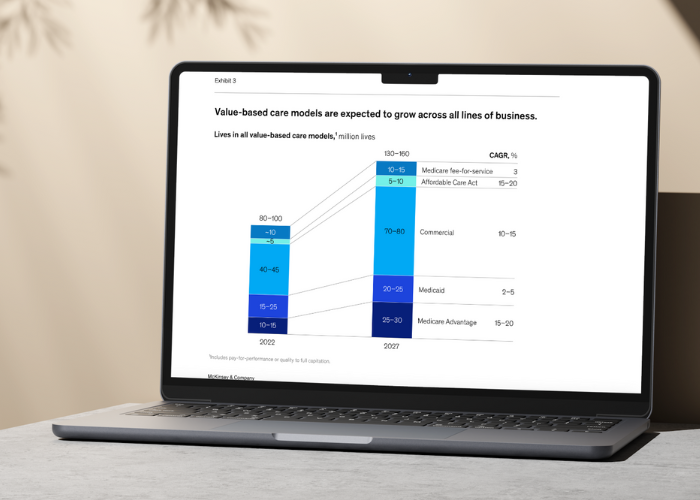
Why VBC is Gaining Traction
VBC champions the patient. By focusing on positive outcomes and overall well-being, patients like Mrs. Smith receive more holistic treatment plans. This could mean a combination of physical therapy, medication, and lifestyle changes instead of another costly and potentially unnecessary MRI.
By focusing on the patient and delivering focused care, the value-based care model is improving breast cancer screening rates by 7% and diabetic care by 8%, all while minimizing emergency department visits by 14%. Furthermore, VBC can be a more economical model in the long run. Initial investments in retraining staff and updating systems might seem hefty, but the potential for savings down the road is significant. Emphasizing preventive care and reducing hospital readmissions can dramatically cut costs. Plus, patients, when treated holistically, tend to stick with their providers, further establishing financial stability for healthcare institutions.
Additionally, with the spotlight on patient satisfaction and quality care, patient engagement naturally soars. The human element returns to the forefront of healthcare. Patients feel valued, listened to, and central to their care plans.
Facilitating the Shift with Digital Transformation
Tech Tools Bridging the Gap
Leveraging technology is the key to a smoother transition to VBC:
- EHR Optimization: Modern Electronic Health Record (EHR) systems tailored to VBC can actively track patient outcomes, ensuring providers get real-time feedback on their care strategies. For example, after analyzing consolidated patient data, a hospital could identify more efficient post-surgery recovery techniques.
- AI & Predictive Analytics: Sophisticated algorithms predict patient needs, allowing providers to be proactive. It's like having a weather forecast for patient health. If potential issues are on the horizon, providers can intervene early, often preventing more significant problems down the line.
- Telemedicine: The recent global health crisis highlighted the value of telemedicine. It’s not only convenient but also reduces unnecessary physical visits, making healthcare more accessible and efficient.
- Interoperability: Seamless communication across platforms ensures that every member of a patient's care team is on the same page. Imagine the seamless care a patient would receive if a specialist in one state could instantly access and understand tests done by a general practitioner in another.
The Roadblocks on the Route to VBC
As with any change to traditional methods and processes, transitioning to value-based care comes with its own obstacles.
The Inevitable Challenges
It's essential to address concerns head-on:
- Transitioning from FFS to VBC requires a complete overhaul of the billing systems we've become accustomed to. It’s akin to learning a new language after speaking only one for years.
- Training is crucial. It's not just about familiarizing teams with a new billing structure but instilling a new philosophy of care. This requires commitment from all levels, from reception staff to top-tier surgeons.
- Evaluating tech ROI becomes paramount. It's vital to continually assess whether the tech investments are fostering better patient care and financial health.
- Keeping up with the ever-changing regulatory landscape is another hurdle. New payment models mean new standards, and compliance can't be compromised.
Charting the Course Ahead
Laying a Robust Foundation
A strategic approach is critical:
- Collaboration is key. Garnering insights from every department ensures a well-rounded transition strategy.
- Test the waters with pilot programs. These can be scaled up once their viability is proven, reducing risk.
- Staying updated on technological advancements and modern trends and innovations in healthcare is non-negotiable. The landscape evolves rapidly, and we must evolve with it.
- Regularly check in on transition progress. Assess what’s working and, importantly, what isn’t. Flexibility can make or break this transition.
Conclusion
The evolution from fee-for-service to value-based care, bolstered by digital transformation, is an exciting paradigm shift in healthcare. In fact, the increasing adoption of the value-based payment model could lead to a valuation of $1 trillion in enterprise value for payers, providers, and investors.
For healthcare leaders, this journey is rife with opportunities and challenges. With a patient-centered mindset and strategic tech integration, providers are not just improving their financial models; they're enriching the lives of those they serve.
Want to learn more about the importance of enabling value-based care? Watch our interview with Microsoft's Amy Berk, MSN RN, Director of Population Health, on The Health/Tech Edge as she discusses the topic of patient data interoperability, the evolution of care delivery models, and the integration of care through partnerships between payers and providers.


.png)

.png)